AGE RELATED MACULAR DEGENERATION (AMD)
AMD is a progressive condition affecting the macula - the central part of the retina that gives us fine detailed vision. With age, there is a slow deterioration of the macula and supporting underlying layer. As a result, central vision declines. AMD is now the most common cause of visual loss in people aged 50 and over, in the western world. There are two main types of AMD, ‘dry’ and ‘wet’.
Dry AMD
The most common form of AMD is known as dry AMD and this accounts for more than 80% of cases. It occurs when light sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye. Although usually only slowly progressive, and frequently mild, it can cause profound visual loss. About 10% of individuals with dry AMD may develop Wet AMD.
Wet AMD
This is far less common but potentially more severe than dry AMD. It is characterised by the growth of abnormal blood vessels (subretinal neovascularisation or SRNV), which leak, causing the retina to lift away from the outer coats of the eye. The macula then becomes swollen and vision is impaired. The earliest feature of wet AMD is an awareness of straight lines becoming distorted. In the later stages, the abnormal blood vessels can haemorrhage, producing dramatic central visual loss. Once vision is destroyed, it cannot be regained.
Managing with AMD
As AMD is not painful, presenting symptoms are sometimes ignored. In its early stages, dry AMD may cause central vision to be blurred or distorted. People with wet AMD will see straight lines as wavy or fuzzy, while those with advanced AMD often notice a blank patch or dark spot in their central vision. Some people see lights, shapes or colours that are not there. These symptoms make it difficult to read or recognise faces. Eventually all central vision may be lost. However, peripheral vision remains and patients can usually maintain independence.
It is often important to carry out investigations, at the time of referral and at regular intervals thereafter, to determine whether you have the dry or the wet form of AMD. These tests may also help decide whether or not the disease is active and treatable. The tests most commonly performed are fundus fluorescein angiography (FFA) and Optical Coherence Tomography (OCT).
FFA involves the injection of a fluorescent yellow dye into a vein in the arm and, as this circulates around the body and eye, flash photographs are taken of the back of the eye. This allows a detailed view of the blood vessels in the retina and at the macula. OCT is a non-invasive test, rather like an ultrasound, but differing in that it that uses a beam of light (rather than sound waves as used in an ultrasound) to produce pictures of the macula. OCT is commonly used to determine the thickness of the macula and the responses to treatment.
Treatments for wet AMD most commonly include the injection into the eye of a special drug referred to as anti-vascular endothelial growth factor (anti-VEGF) and, sometimes, Photodynamic Therapy (PDT).
LUCENTIS OR AVASTIN (Anti-VEGF Drugs)
The aim of treatment with these drugs is to prevent further loss of vision although some fortunate patients have actually regained some vision following the use of these drugs. A tiny quantity of fluid containing the drug is injected into the vitreous, a jelly-like substance in the middle of the eye, after the eye has been numbed with anaesthetic drops. These drugs need to be injected into the eye at regular intervals (about every 4-6 weeks). How long this is continued for depends on the individual patient’s clinical circumstances. These injections should ideally be given in an Operating Theatre, to minimise the risk of potentially serious infection.
For more information on AMD and Avastin click on the link below:
http://www.loveyoureyes.org.uk/content/view/12/33/
PHOTODYNAMIC THERAPY (PDT)
During PDT a special dye called Visudyne® is injected into an arm vein. A special contact lens is placed on the eye. A special laser is then applied to the eye which activates the dye within the abnormal macular blood vessels with the aim of destroying them.
Treatment for wet AMD can halt the condition’s progress, but cannot replace lost vision. It is common for a cataract to co-exist with AMD and, whilst cataract extraction may do little to help reading vision, the improved illumination following surgery can provide a substantial benefit to overall visual function.
Does AMD lead to blindness?
AMD almost never leads to total blindness because only the central retina is affected. However, if left untreated, it can result in only outer peripheral vision remaining, with black holes or dim images at the centre.
Is there anything I can do to avoid AMD?
People over the age of 40 should have regular eye tests every 1 to 2 years. Reducing the risk factors by eating a healthy diet, keeping blood pressure down and stopping smoking can all help prevent AMD.
What are the symptoms of dry AMD?
The most common symptom is slightly blurred vision. You may have difficulty recognising faces and need more light for reading and other tasks. Dry AMD generally affects both eyes, but vision can be lost in one eye while the other eye seems unaffected.
What are the symptoms of wet AMD?
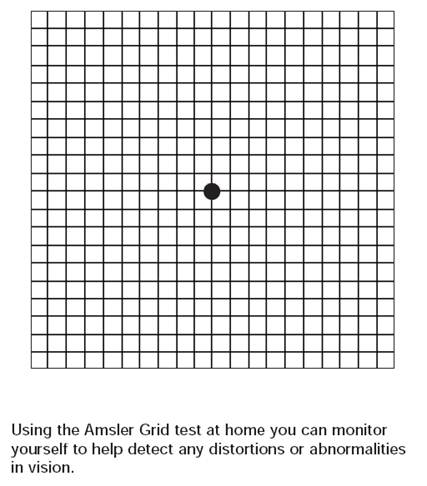
Distortion of central vision with straight lines appearing wavy are the cardinal symptoms. Change should be reported as a matter of urgency as the success of treatment depends upon prompt intervention.
Do I need to have any special tests?
It is sometimes necessary to carry out investigations both initially and at regular intervals to determine whether you have the dry or wet form of AMD, whether the macula changes are active or not and whether or not treatment is appropriate. The most commonly requested tests are fundus fluorescein angiography (FFA) and Optical Coherence Tomography (OCT).
During FFA a fluorescent yellow dye injected into a vein in the patient's arm circulates around the body and eye, and flash photographs are obtained through dilated pupils. FFA provides a detailed view of the blood vessels at the macula.
OCT is a non-contact test, analogous to ultrasound but using light instead of sound, to image the macula by means of cross-sectional images. OCT can be very useful to determine the presence or absence of fluid, objectively determine the retinal thickness and also assess the response to treatment.
Is there any treatment for Dry AMD?
There is no actual treatment for dry AMD, but it is advised to reduce risk factors such as smoking and high blood pressure. You should protect your eyes from exposure to harmful sunlight by wearing sunglasses outdoors, and eat a diet rich in foods containing antioxidants and naturally occurring pigments, such as those found in brightly coloured vegetables like peppers, broccoli and spinach. Scientific studies have shown that, if caught in the early stages, high doses of vitamins A, C and E (together with zinc) can substantially lower the risk of both worsening of dry disease and the development of wet AMD. It is common now for these vitamin preparations to be supplemented with the protective pigments lutein and zeoxanthin. These measures are more relevant for those individuals with certain types of early AMD and for those who have a family history of the condition.
Your ophthalmic consultant will be able to advise you.
It is common for a cataract to co-exist with AMD and, whilst cataract extraction may do little to help reading vision, the improved illumination following surgery can provide a substantial benefit to overall visual function.