The term corneal dystrophy refers to an abormality in the structure of the cornea (the clear front window of the eye). These abnormalities of structure are a group of genetic, often progressive, eye conditions in which abnormal material often deposits in the clear cornea. Corneal dystrophies may be asymptomatic in some individuals whilst in others they can cause significant vision impairment.
The different forms of corneal dystrophy are typified by differing age of onset and symptoms. There are some common characteristics; most forms of corneal dystrophy are bilateral, affecting both eyes. They are slowly progressive, do not affect other areas of the body, and tend to run in families.
Corneal dystrophies cause problems because of the accumulation of abnormal material within the cornea. The cornea serves two functions; it protects the rest of the eye from dust, germs and other harmful or irritating material, and it acts as the eye’s first focussing structure, bending incoming light onto the lens, where the light is then further focussed onto the retina (the layer of light-sensitive cells lining the back of the eye). The retina processes the light, coverting it to images, which are then transmitted to the brain. The cornea needs to be clear & transparent so that it can focus light entering the eye.
The cornea is made up of five layers:
- the epithelium, the outer protective layer of the cornea
- Bowman membrane, this second tough layer is difficult to penetrate
- stroma, the thickest layer of the cornea, consisting mainly of water & collagen fibers
- Descemet’s membrane, a thin, strong inner layer
- endothelium, the innermost layer made up of specialised cells that pump excess water out of the cornea.
Corneal dystrophies are characterised by the accumulation of foreign material in one or more of the these layers.
A symptom common to many forms of corneal dystrophy is recurrent corneal erosion, in which the outermost layer of the cornea (epithelium) does not stick to the eye properly. Recurrent corneal erosion can cause discomfort or severe pain, an abnormal light sensitivity, a foreign body sensation in the eye, and blurred vision.
Some examples of corneal dystrophies are listed below:
ANTERIOR CORNEAL DYSTROPHIES
These conditions affect the outer layers of the cornea including the epithelium, the epithelial basement membrane (a thin membrane that separates epithelial cells from underlying tissue), and the Bowman membrane.
Epithelial Basement Membrane Dystrophy
This is characterised by the development of very tiny dots (microcysts), gray areas that resemble the outlines of countries on a map, or fine lines that resemble fingerprints on the epithelial layer of the cornea. Most individuals are asymptomatic but sometimes symptoms can include recurrent erosions and blurred vision. This common form of corneal dystrophy is also known as map-dot-fingerprint dystrophy or Cogan microcystic dystrophy.
Meesmann Corneal Dystrophy
This is a very rare form of corneal dystrophy, affecting the epithelial layer. It is characterised by clusters of multiple, small, clear cysts which are roughly the same size. Affected individuals may experience mild irritation and a slight decrease in clarity of vision. Photophobia (light sensitivity) and excessive tear formation can occur in this condition.
Lisch Corneal Dystrophy
This rare form of dystrophy is characterized by clusters of multiple, tiny cysts or lesions, band-shaped or spiraled (whorled) in appearance. In some cases, affected individuals do not have any symptoms. Some individuals may have decreased clarity of vision, and double vision affecting only one eye (monocular diplopia).
Reis-Buckler Corneal Dystrophy
This form affects the Bowman membrane and is characterized by clouding (opacity) and progressive scarring of the membrane. During the first decade of life, affected individuals may initially develop recurrent erosions that cause significant pain. Recurrent erosions may eventually stabilize as affected individuals grow older. Additional symptoms may develop including photophobia, a sensation of a foreign body in the eye, and a reduction in clarity of vision often by late teenage years.
Thiel-Behnke Corneal Dystrophy
This form of corneal dystrophy also affects the Bowman membrane and may be very difficult to distinguish from Reis-Buckler corneal dystrophy. The abnormalities affecting the cornea may resemble honeycombs. Recurrent corneal erosions begin during childhood, but visual acuity is not affected until later life. Pain and photophobia may also occur.
STROMAL CORNEAL DYSTROPHIES
These corneal dystrophies affect the central layer of the cornea. Some of them can progress to affect other layers of the cornea.
Granular Corneal Dystrophy Type I
This is characterised by the development of small particles that collectively resemble breadcrumbs, and these lesions slowly grow eventually combining to form larger lesions. Individuals may develop recurrent erosions. Although vision is usually unaffected early in the disease, decreased visual acuity may occur by the fourth or fifth decade.
Granular Corneal Dystrophy Type II
In granular corneal dystrophy type II, (Avellino corneal dystrophy), lesions develop on the stroma usually in the first or second decade of life. The opacities resemble a cross between the granular lesions of granular corneal dystrophy type 1 and lattice lesions of lattice corneal dystrophy (see below). With age, the lesions may become larger, more prominent and involve the entire stromal layer. Some older individuals have decreased clarity of vision due to haze (clouding of the cornea). Recurrent erosions may develop in some cases.
Lattice Corneal Dystrophy
Lattice corneal dystrophies are a common form of stromal dystrophy and two main variants have been identified. They are characterised by the development of lesions that form branching lines resembling cracked glass. Lattice dystrophy type I usually occurs by end of the first decade. Recurrent corneal erosions (which can be painful) often precede these characteristic changes to the stroma. Affected individuals may have decreased clarity of vision and photophobia.
Gelatinous droplike corneal dystrophy, also known as familial subepithelial corneal dystrophy, develops in individuals during the first decade of life and is characterized by loss of vision, an abnormal sensitivity to light), excessive tearing, and the feeling of foreign substances in the eye. Gelatinous masses of amyloid, a type of protein, accumulate beneath the corneal epithelium and make the cornea opaque, progressively impairing vision.
Macular Corneal Dystrophy
Individuals with this form of corneal dystrophy are born with clear corneas, but eventually develop clouding of the stroma, usually between 3-9 years of age. Progression of the lesions results in decreased visual acuity and irritation early during life. Sometimes, significant vision loss can occur by the second decade. Severe vision loss may develop by the third or fourth decade.
POSTERIOR CORNEAL DYSTROPHIES
These dystrophies affect the innermost layers of the cornea including Descemet’s membrane and the endothelium. These are the layers of the cornea closest to the inner structures of the eye. These disorders can potentially affect all layers of the cornea.
Fuchs Endothelial Dystrophy
 This dystrophy usually develops during middle age, although there may be no symptoms initially. Fuchs dystrophy is characterized by problems with tiny endothelial cells which have the crucial function of pumping water out of the cornea and back into the eyeball.
This dystrophy usually develops during middle age, although there may be no symptoms initially. Fuchs dystrophy is characterized by problems with tiny endothelial cells which have the crucial function of pumping water out of the cornea and back into the eyeball.
In Fuchs dystrophy these cells deteriorate and the cornea fills with water and swells. The swelling associated blurred vision are worse in the morning, but gradually improve throughout the day. Tiny blisters may form on the cornea, eventually rupturing and causing extreme pain.
Affected individuals may also have a gritty/sandy feeling within the eye, be abnormally sensitive to light and see a glare or halos. As the disease progress, vision no longer improves during the day and significant vision loss may occur, possibly requiring corneal transplant surgery.
Posterior Polymorphous Dystrophy
This uncommon form of corneal dystrophy can present at birth (with clouding of the cornea) or later during life and is characterized by lesions affecting the endothelium. Most individuals do not develop symptoms. Effects on the cornea may be slowly progressive. Although usually bilateral, the severity of the condition can be very asymmetric. In severe cases, individuals may develop swelling of the stroma, photophobia, decreased vision, and the feeling of foreign material in the eye. Rarely, increased pressure within the eye may occur.
Causes
Most cases of corneal dystrophy are inherited as an autosomal dominant trait with variable expressivity.
Genetic diseases are determined by the combination of genes for a particular trait that are on the chromosomes received from the father and the mother. In dominant conditions, only one abnormal gene copy is required, whereas with recessive conditions, both copies of the gene need to be defective. The dominant gene can be passed down from either parent.
The term variable expressivity means that some individuals who inherit the same gene for a dominant disorder may not have the degree of the condition..
Who is Affected?
Most corneal dystrophies affect women and men equally. One main exception is Fuchs corneal dystrophy which affects women about four times as often as men. The corneal dystrophies can affect individuals of any age. Since many affected people are asymptomatic, it is difficult to know how many people actually have corneal dystrophies.
Diagnosis
The presence of a corneal dystrophy may be found incidentally during a routine eye examination. A diagnosis may be confirmed by a thorough clinical evaluation, a detailed patient history and a variety of tests, such as a slit lamp examination, in which a special microscope (slit lamp) allows a physician to view the eye through high magnification. Some specific corneal dystrophies can be diagnosed with molecular genetic tests even before symptoms develop.
The treatment of corneal dystrophies varies. Individuals who are asymptomatic, or only have mild symptoms, may not require any treatment. They can, instead, be regularly observed to detect potential progression of the disease.
Other corneal dystrophies may need treatments including eye drops, ointments, lasers and corneal transplant. Recurrent corneal erosions (a common finding in most corneal dystrophies) may be treated with lubricating eye drops, ointments, antibiotics or specialized (bandage soft) contact lenses. If recurrent erosions persist, additional measures may be necessary.
Some conditions, such as epithelial dystrophies or granular dystrophy, may benefit from Excimer laser photherapeutic keratectomy, where available.
For other individuals where laser treatment is not possible and the symptoms are significant, a corneal transplant may be necessary.
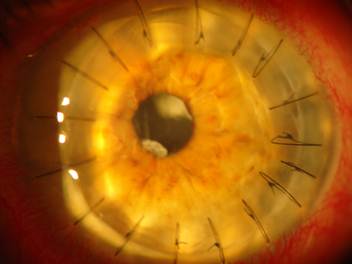
Corneal transplants can be very successful in treating individuals with severe forms of corneal dystrophies. However, patients need to be aware that the dystrophic changes will eventually develop in the donated “new” cornea.
Recent advances in corneal transplant surgery have made partial thickness, or lamellar, transplant surgery much more commonplace
The exact treatment option chosen will depend upon various factors including
- what is the specific type of corneal dystrophy presen
- the severity of associated symptoms
- the rate of progression of the disease
- patient’s overall health and quality of life.
Genetic counseling may also be of benefit for affected individuals and their families.